Spondyloarthritis of the vertebral ankylosis: Symptoms at the sacroiliac joint and their management
In the realm of joint disorders, two conditions that often cause pain and inflammation in the sacroiliac (SI) joint are osteoarthritis (OA) and ankylosing spondylitis (AS). While both can cause discomfort, it's essential to understand the key differences between these two conditions to ensure accurate diagnosis and effective treatment.
Ankylosing spondylitis (AS) is a type of arthritis that can affect the sacroiliac joint. This condition is an autoimmune inflammatory disorder, where the immune system attacks the joint, leading to inflammation, pain, and potential joint fusion (ankylosis). In contrast, osteoarthritis (OA) in the SI joint is primarily a degenerative wear-and-tear disease, characterised by cartilage breakdown and joint deterioration, leading to pain and stiffness often localised and worsened by mechanical stress.
The symptoms and clinical features of these two conditions differ significantly. Osteoarthritis SI joint pain is often mechanical, worsening with activity such as standing, climbing stairs, or prolonged walking, and may include stiffness with use. On the other hand, AS sacroiliitis causes inflammatory pain that is often worse at rest or at night, is associated with morning stiffness that improves with activity, and may be bilateral and symmetric. Systemic features such as progression to spinal fusion are also typical in AS.
The onset and progression of these conditions also differ. Osteoarthritis develops gradually with age or joint strain, whereas AS often presents in younger adults with chronic inflammatory symptoms and has a progressive course involving the spine.
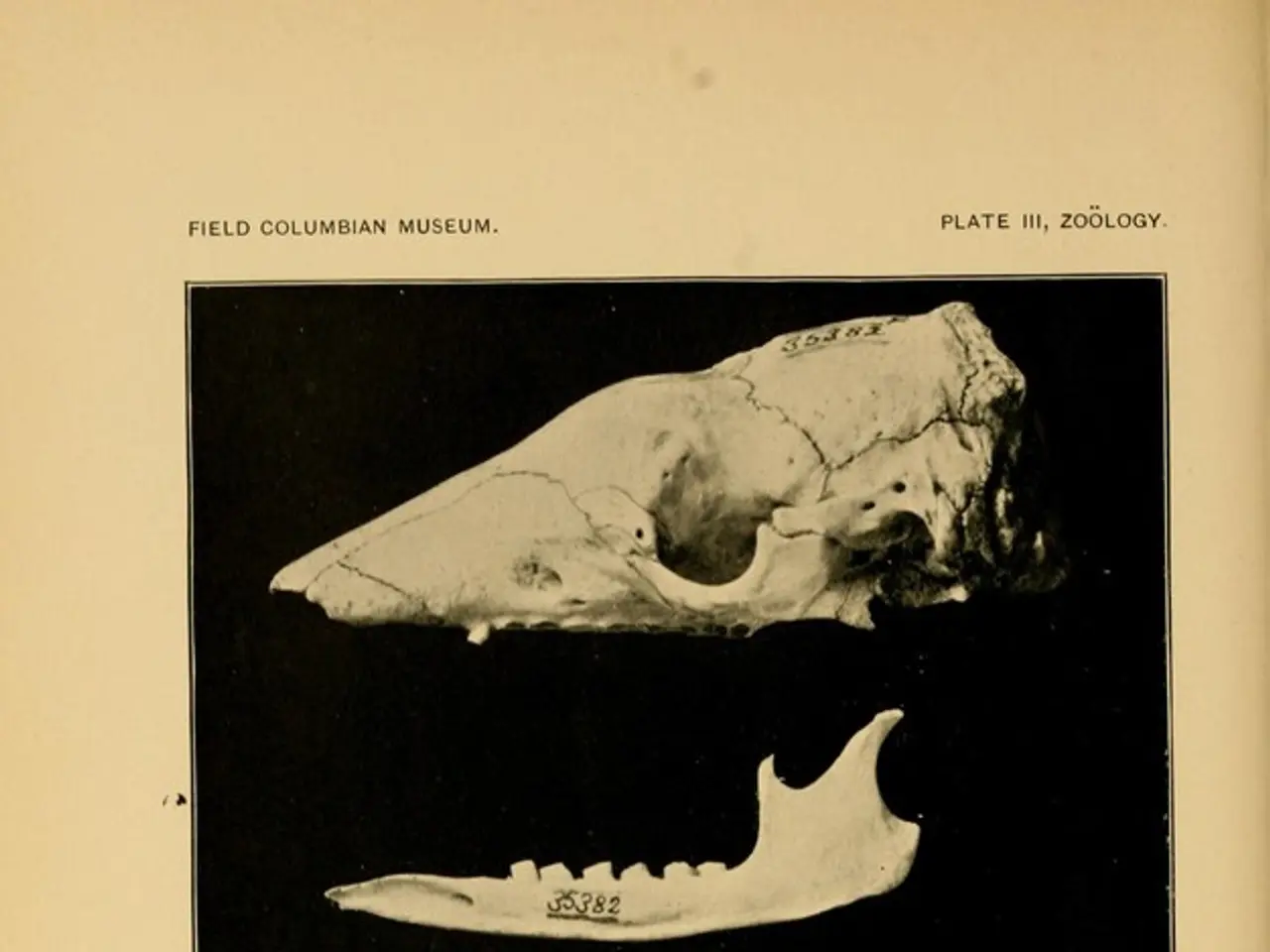
Imaging findings also help differentiate between the two conditions. Osteoarthritis shows degenerative changes such as joint space narrowing and osteophyte formation on imaging, while AS shows sacroiliitis with erosions, sclerosis, and, eventually, fusion of the SI joints visible on X-ray or MRI, reflecting inflammation and new bone formation.
Doctors can grade inflammation of the SI joint using the modified New York criteria, which includes clinical and radiological criteria. For a doctor to diagnose AS, sacroiliitis must be at least grade 2 on both sides or at least grade 3 on one side, and the individual must have at least one of the following clinical criteria: lower back pain for at least 3 months that improves with exercise but not with rest, limited lower spine flexibility, or limited lower chest expansion.
While both conditions can cause SI joint pain and inflammation, osteoarthritis reflects degenerative changes localised to the SI joint surfaces, whereas ankylosing spondylitis involves systemic autoimmune inflammation causing sacroiliitis with potential joint fusion. Recognition of these differences is important for diagnosis and management.
It's important to note that AS may also affect other parts of the body, such as the shoulders, hips, ribs, hands, heels, and feet. In severe cases, an individual with AS may need surgery to replace a joint that has significant damage, such as the hip or knee.
For those concerned about their risk of developing conditions associated with AS, it's recommended to discuss this with a doctor, who can provide advice on ways to reduce these risks. Physical therapy can help a person improve their muscle strength and maintain mobility in their spine and other joints.
In conclusion, while both osteoarthritis and ankylosing spondylitis can cause discomfort in the SI joint, understanding the differences between these two conditions is crucial for accurate diagnosis and effective treatment. If you are experiencing persistent SI joint pain or inflammation, it's advisable to consult with a healthcare professional.