Potential Adverse Reactions to Prolia: An Overview and Guidelines for Coping
Prolia, a monoclonal antibody used to treat osteoporosis and bone thinning, has been shown to be effective for many postmenopausal women. However, like any medication, it comes with potential side effects that patients should be aware of [1][2][3][5].
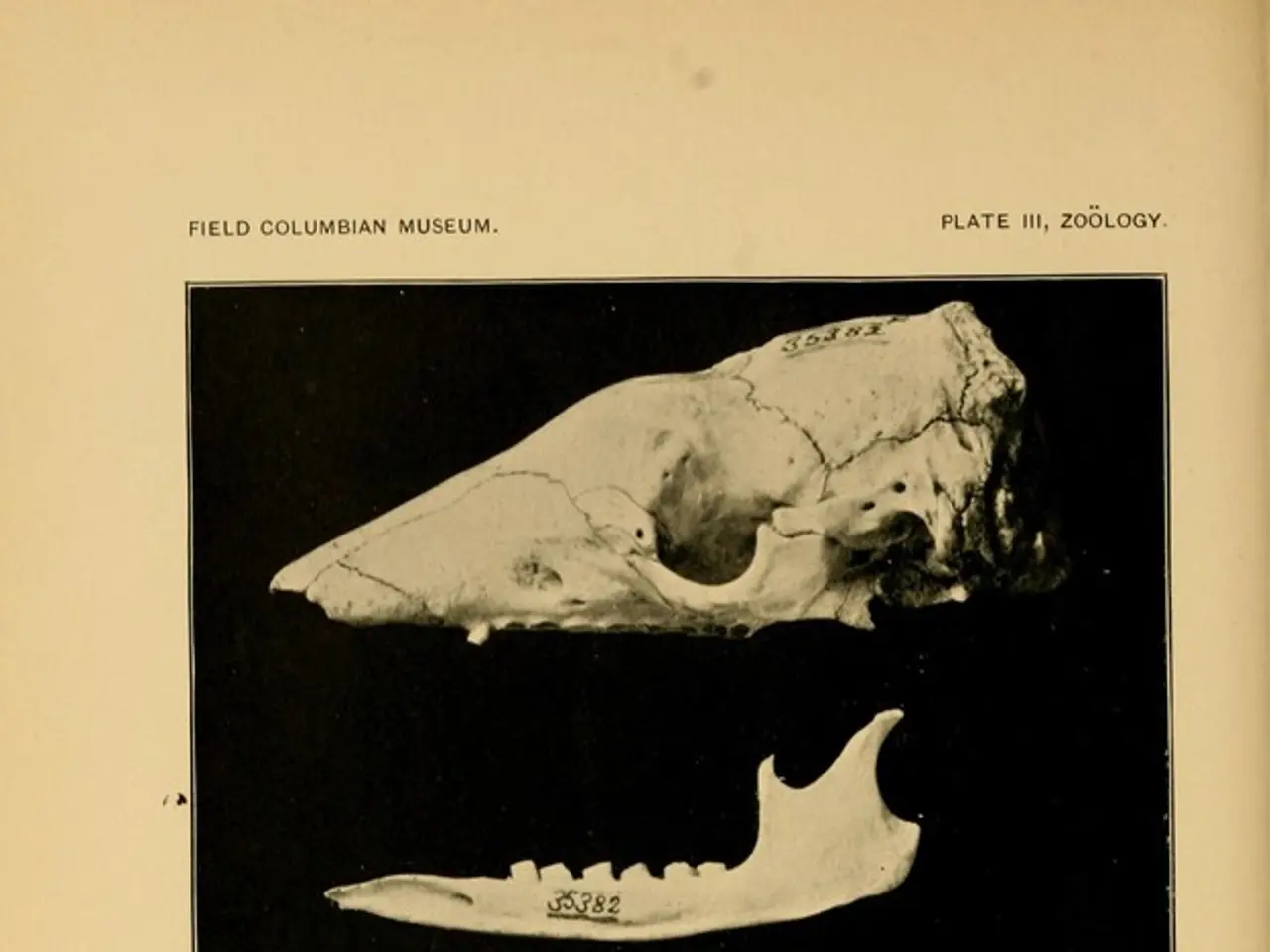
One of the most serious side effects reported with Prolia is the rare but serious event of osteonecrosis of the jaw (ONJ), a condition involving breakdown of jaw bone tissue. This requires regular dental check-ups during treatment to mitigate the risk [1][5].
Another potential risk is the occurrence of atypical femoral fractures, unusual fractures of the thigh bone, which may be associated with prolonged antiresorptive therapy [1][5].
Patients with advanced chronic kidney disease are at higher risk of severe hypocalcemia, a condition characterised by low blood calcium levels. It's essential that calcium levels are corrected before and monitored during treatment [2].
Clinical trials have reported a higher frequency of serious infections, such as skin infections and endocarditis, leading to hospitalizations in Prolia-treated patients compared to placebo [3][5].
Upon stopping Prolia, there is a notable rise in bone turnover markers and a risk of multiple vertebral fractures within about 7 to 19 months. Transitioning to another therapy is recommended to manage this risk [3][5].
Common mild side effects include muscle and bone aches and pains, dizziness, high cholesterol levels, bladder or urinary tract infections, common cold symptoms, bronchitis, headache, pain in the upper abdomen, sciatica, peripheral edema, itching, constipation, and joint pain [1][5].
It's important to note that Prolia may increase the risk of falling if you drink too much alcohol, especially if you have osteoporosis. Maintaining good oral hygiene during treatment, including regular professional dental cleanings, is also recommended [4].
The active ingredient in Prolia is denosumab. If you notice any tooth or jaw pain, or sensitivity while using Prolia, it's crucial to talk with your doctor or dentist right away [2].
While your doctor will monitor your cholesterol levels with regular blood tests, it's important to understand that some side effects may not be reversible, and they may continue for as long as the medication is taken [6].
Overall, Prolia is considered effective and safe for many postmenopausal women with osteoporosis, but long-term use demands careful monitoring to detect and manage rare serious adverse effects and to plan for safe discontinuation [1][2][3][5].
References: [1] National Osteoporosis Foundation. (2021). Prolia. Retrieved from https://www.nof.org/patients/treatment/medication-therapy/prolia/ [2] Drugs.com. (2021). Prolia. Retrieved from https://www.drugs.com/prolia.html [3] Mayo Clinic. (2021). Prolia (denosumab). Retrieved from https://www.mayoclinic.org/drugs-supplements/prolia-denosumab/description/drg-20073545 [4] FDA. (2012). FDA Drug Safety Communication: FDA warns about increased risk of certain infections, including some that can be life-threatening, with Prolia and Xgeva. Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-about-increased-risk-certain-infections-including-some [5] NHS. (2021). Prolia. Retrieved from https://www.nhs.uk/medicines/prolia/ [6] MedlinePlus. (2021). Prolia. Retrieved from https://medlineplus.gov/druginfo/meds/a605008.html
- Prolia, a treatment for osteoporosis and bone thinning, has been shown effective for many postmenopausal women, but it comes with potential side effects.
- One serious side effect associated with Prolia is osteonecrosis of the jaw (ONJ), a condition involving jaw bone tissue breakdown.
- Regular dental check-ups are necessary during Prolia treatment to reduce the risk of ONJ.
- Another risk is the occurrence of atypical femoral fractures, unusual thigh bone fractures, possibly linked to prolonged antiresorptive therapy.
- Patients with advanced chronic kidney disease face a higher risk of severe hypocalciemia, a condition marked by low blood calcium levels, during Prolia treatment.
- clinical trials have shown a higher frequency of severe infections, including skin infections and endocarditis, in Prolia-treated patients compared to placebo cases.
- After stopping Prolia, there's an increased risk of multiple vertebral fractures within about 7 to 19 months, necessitating a transition to another therapy.
- Common mild side effects include muscle and bone aches, dizziness, high cholesterol, bladder or urinary tract infections, common cold symptoms, bronchitis, headache, abdominal pain, sciatica, peripheral edema, itching, constipation, and joint pain.
- Alcohol consumption and osteoporosis may increase the risk of falls while taking Prolia, making maintaining good oral hygiene, including regular professional dental cleanings, essential.
- The active ingredient in Prolia is denosumab, and tooth or jaw pain or sensitivity should be reported immediately to a doctor or dentist.
- Prolia's long-term use demands careful monitoring to manage rare serious adverse effects and safe discontinuation.
- While your doctor will monitor cholesterol levels, some side effects may continue for the duration of the medication.
- Prolia is generally considered effective and safe for postmenopausal women with osteoporosis, but its long-term effects on other medical conditions like depression, COPD, diabetes, Alzheimer's, obesity, or neurological disorders are not well-understood.
- The impact of Prolia on eye health, hearing, health and wellness, climate change, mental health, skin care, and women's health issues like menopause and migraines is also not known.
- The effectiveness and safety of Prolia for type-2 diabetes, psoriasis, and other skin conditions have not been established through clinical trials.
- Prolia may offer potential benefits for health and wellness, but its long-term effects on chronic diseases, environmental science, and space and astronomy remain to be seen.