Mouth bacteria's potential connection to memory loss and dementia risk
In a groundbreaking development, researchers at the University of Exeter have discovered that specific bacteria living in the mouth can significantly impact cognitive function. This finding opens up a potential non-invasive screening method for dementia risk through routine dental checkups.
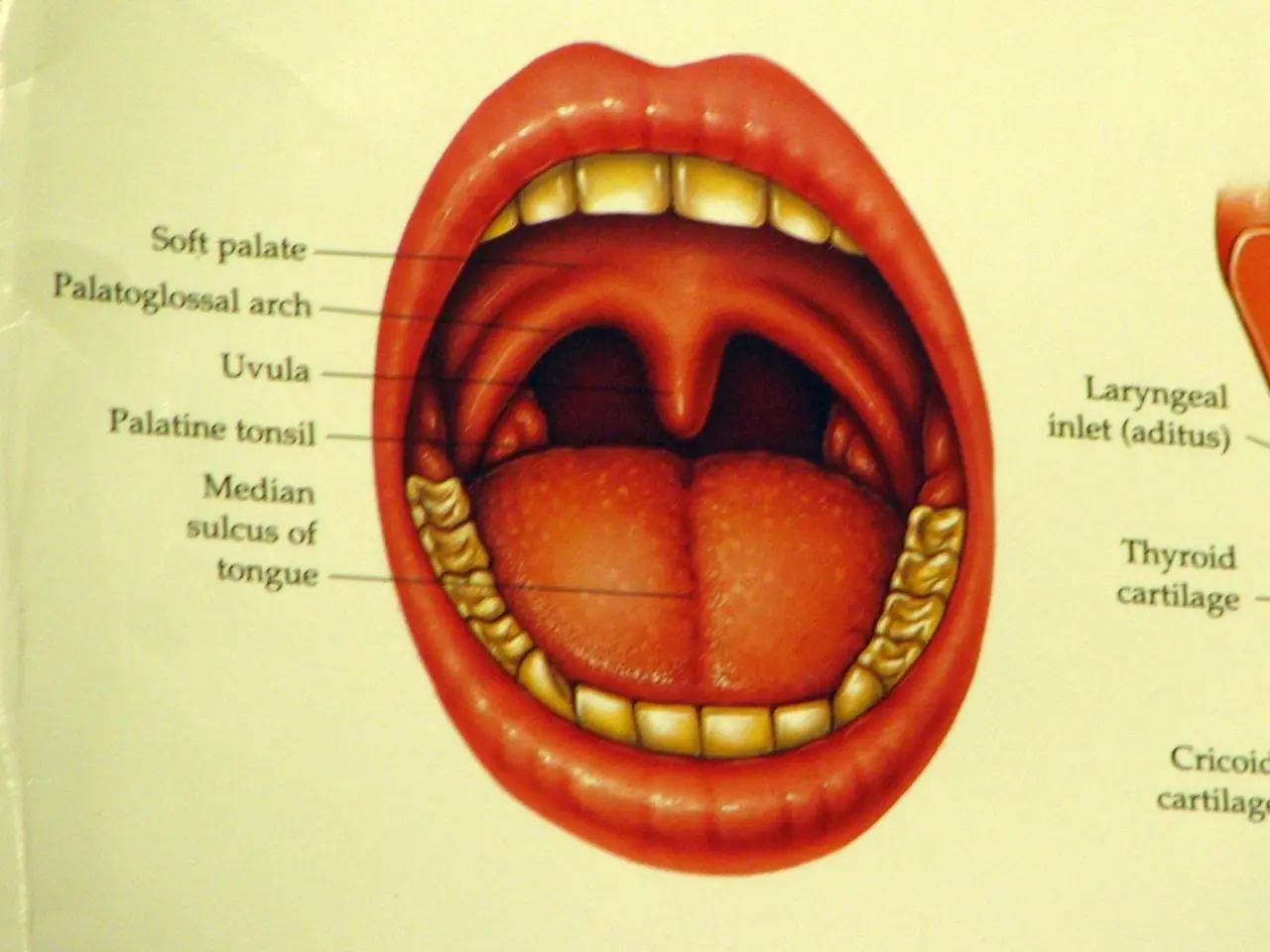
The study sheds light on the role of nitric oxide in the relationship between oral bacteria and brain function. The oral microbiome, a diverse community of microorganisms in the mouth, influences brain health primarily by modulating neuroinflammation, systemic inflammation, and central nervous system signaling.
Imbalances in the oral microbiome, known as oral dysbiosis, can lead to harmful effects such as neuroinflammation that are linked to brain disorders including Alzheimer's disease, Parkinson’s disease, multiple sclerosis, depression, and anxiety. Pathogenic oral bacteria can enter the bloodstream, reach the brain, and trigger immune responses that impair neuronal function and contribute to neurodegeneration.
For instance, periodontal pathogens like Porphyromonas gingivalis produce toxins and virulence factors (gingipains) that exacerbate neuroinflammation and promote Alzheimer's characteristic pathology such as amyloid-beta plaque formation. Oral dysbiosis is also associated with disrupted blood-brain barrier integrity and altered brain metabolites, suggesting a direct impact on brain chemistry and neurodevelopment.
The good news is that potential strategies to modify the oral microbiome for brain health are within reach. These include maintaining or restoring a balanced oral microbial ecosystem through routine dental cleanings and periodontal disease management, use of probiotics, tongue scraping, antimicrobial mouth rinses, fluoride treatments, dental sealants, consistent oral hygiene practices, and dietary recommendations that promote oral microbiome balance.
As the World Health Organization projects that dementia cases will triple by 2050, affecting over 150 million people worldwide, the importance of these preventive measures cannot be overstated. By addressing oral health, we may be able to mitigate the risk of cognitive decline and related disorders.
Moreover, nitric oxide, a molecule crucial for brain function and memory formation, plays a vital role in memory formation and retention. As we age, the endogenous pathway for nitric oxide production becomes less efficient, making the nitrate-nitrite-NO pathway increasingly important. Certain oral bacteria are particularly efficient at converting dietary nitrate to nitrite, essentially serving as "nitrate factories" that support NO production.
In summary, a balanced oral microbiome supports brain health by preventing neuroinflammation and systemic inflammation, while dysbiosis can contribute to neurodegenerative and mood disorders. By prioritising oral hygiene, professional dental care, and lifestyle modifications, we can optimise the oral microbiome in support of brain health.
Dental practitioners play a key role in educating patients about these prevention and treatment practices to protect both oral and brain health. With this newfound knowledge, we are one step closer to a future where routine dental checkups could become a valuable tool in the early detection and prevention of cognitive decline.
- The study on oral bacteria and brain function suggests a link between specific medical-conditions, such as dementia, chronic diseases like Alzheimer's and Parkinson’s, mental health issues like depression and anxiety, and the health-and-wellness of the mouth.
- By focusing on maintaining a balanced oral microbiome through regular dental checkups, oral hygiene practices, and potential strategies like probiotics and antimicrobial mouth rinses, dental practitioners can help mitigate the risk of cognitive decline and related disorders.