Lung Fluid Build-up: Origins, Signs, and Further Details
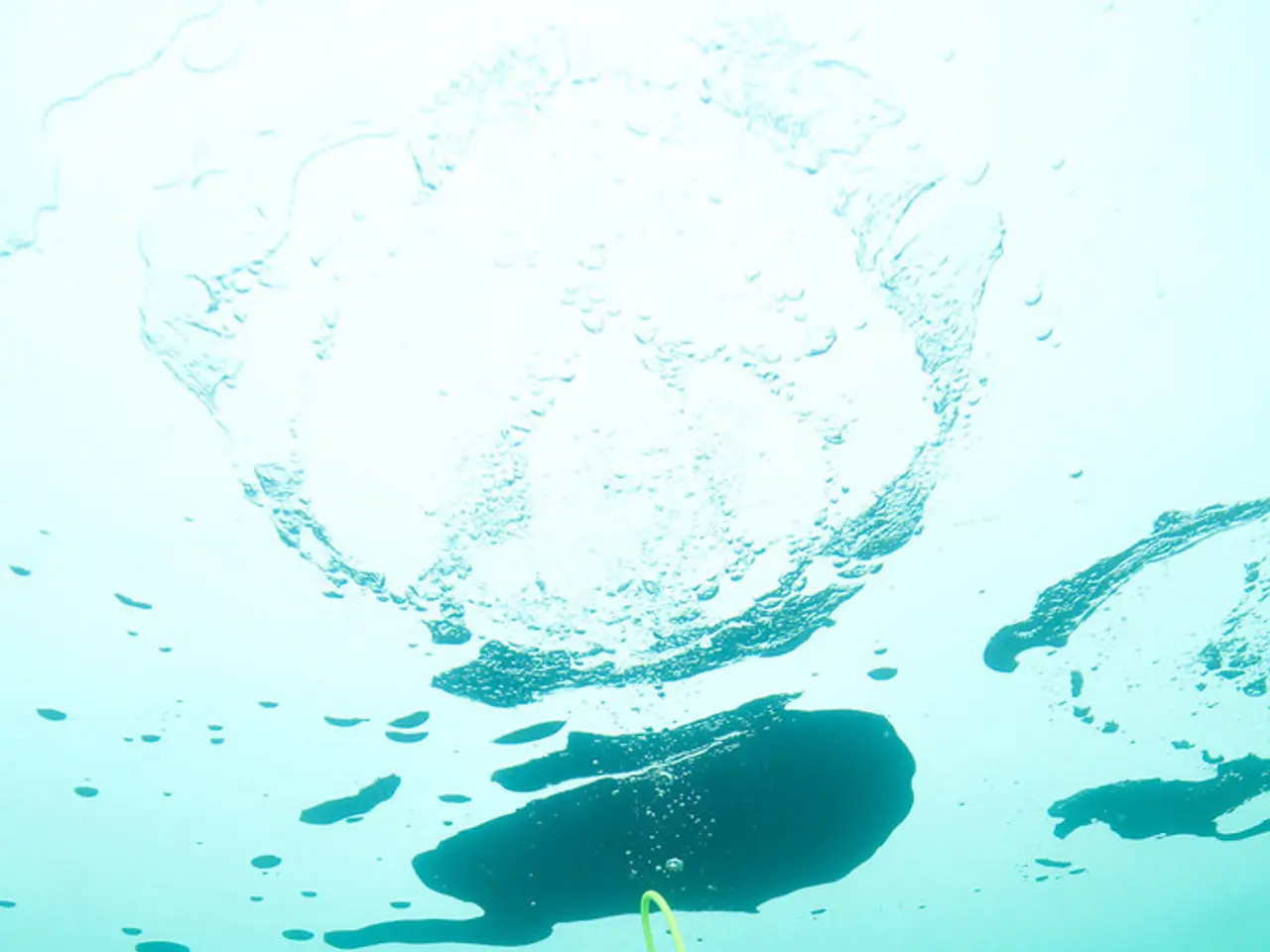
Pulmonary edema, a condition characterised by the accumulation of fluid in the air sacs of the lungs, can be a medical emergency. It's important to distinguish it from related conditions, such as pneumonia, as they are separate but can overlap.
Pulmonary edema is caused by fluid in the lungs, whereas pneumonia is a respiratory infection. Understanding the causes of pulmonary edema is crucial, as treatment strategies vary significantly.
Prevention measures for pulmonary edema include following a doctor's advice, maintaining a healthy, balanced diet, regular exercise, reducing salt intake, lowering cholesterol levels, and quitting smoking. In severe cases, a breathing tube in the trachea and a ventilator may be necessary. Diuretics are often used to help reduce fluid buildup by increasing urine production.
There are two main types of pulmonary edema: cardiogenic and non-cardiogenic. Cardiogenic pulmonary edema is primarily caused by heart-related problems, such as heart failure, heart attack, or coronary heart disease. In contrast, non-cardiogenic pulmonary edema is caused by a variety of factors, including acute respiratory distress syndrome (ARDS), kidney failure, pulmonary embolism, pneumonia, major chest-wall injury, high-altitude exposure, drug overdose, smoke inhalation, viral infections, aspiration during vomiting, neurogenic causes such as stroke or head injury, and more.
The key difference between cardiogenic and non-cardiogenic pulmonary edema lies in their underlying causes and pathophysiology. Cardiogenic edema is caused by heart dysfunction, leading to fluid leakage due to high hydrostatic pressure in vessels, while non-cardiogenic edema is caused by increased capillary permeability due to lung injury, allowing fluid to leak into the alveoli despite normal heart function.
Diagnosing pulmonary edema typically involves a physical exam, listening to the lungs and heart with a stethoscope, blood tests to determine blood oxygen levels, check electrolyte levels, kidney function, liver function, blood counts, and blood markers of heart failure, an echocardiogram or an electrocardiogram (EKG) to determine the condition of the heart, a chest X-ray or a lung ultrasound to check for fluid in or around the lungs and the size of the heart, and possibly a CT scan for further examination.
Symptoms of acute pulmonary edema include shortness of breath, cough, excessive sweating, anxiety and restlessness, feelings of suffocation, pale skin, wheezing, rapid or irregular heart rhythm, chest pain, and rapid weight gain. It's essential to seek immediate medical attention if experiencing these symptoms, as acute pulmonary edema is a medical emergency.
Treatment for pulmonary edema focuses on improving respiratory function and addressing the source of the problem. This may involve administering oxygen through a face mask or nasal cannulas, IV medications to help reduce fluid volume and regulate blood pressure in cases of pulmonary edema caused by circulatory system problems, and other medications such as vasodilators, calcium channel blockers, inotropes, morphine, and medications to reduce anxiety and shortness of breath.
In conclusion, understanding the differences between cardiogenic and non-cardiogenic pulmonary edema is vital for effective treatment. Prevention and early recognition can significantly improve outcomes for those affected by this potentially life-threatening condition.
- Ulcerative colitis, a type of inflammatory bowel disease, shares some similarities with lung conditions, as both can lead to health-and-wellness concerns.
- Predictive science could aid in early detection of diabetes, heart failure, and even cancer, potentially saving lives by enabling prompt treatment-seekers to address these medical-conditions.
- Depression, a common comorbidity in patients with lung diseases like pneumonia, can aggravate symptoms and hinder recovery, making it essential to address mental health alongside physical conditions.
- Hepatitis, a liver disease that can manifest with symptoms such as fatigue, nausea, and jaundice, can be a complicating factor in cases of pulmonary edema.
- AQ, a promising air quality index, is designed to help monitor and alert people about harmful pollutants that may exacerbate lung conditions, such as asthma or COPD.
- In addition to pulmonary edema, medical-conditions like lung cancer, lung fibrosis, and interstitial lung disease can also cause difficulty breathing, necessitating careful and targeted treatment.
- An otherwise healthy lifestyle, characterized by a balanced diet, regular exercise, avoidance of excessive salt and cholesterol, and abstinence from smoking, can help prevent a variety of medical-conditions like diabetes, heart failure, and colitis.
- Medical-conditions like diabetes, heart failure, cancer, hepatitis, and respiratory illnesses (such as pneumonia and pulmonary edema) are complex, requiring a holistic approach to management that considers both prevention and treatment strategies.